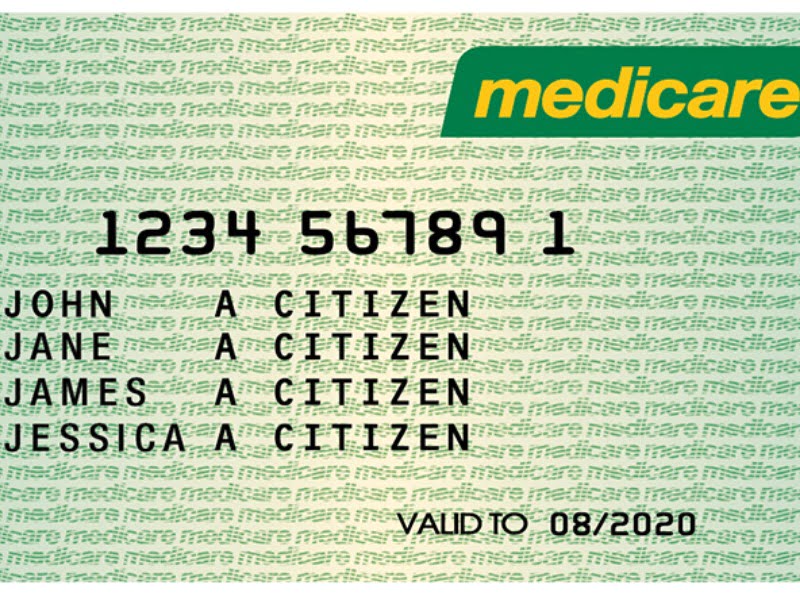
The federal government has unveiled a Medicare data-matching scheme to find fraudulent claims, but is at pains to say it won’t be a repeat of the controversial robodebt program.
It released a consultation guide for the Health Legislation Amendment (Data-matching) Bill 2019 which would allow for data-matching on health information between government departments and agencies, and even private health insurers.
While proposed scheme looks similar to Centrelink’s data-matching regime – which will soon have its legality tested as part of a class action lawsuit – the government says the proposed scheme would not involve any new automation and would be implemented by humans.
This is in stark contrast to robodebt, which involves a mostly automated process where debt letters and please explain notices are sent to welfare recipients if an algorithm detects a potential payment discrepancy. The system has shown to be wrong at least 20 per cent of the time, and places the onus on the recipient to prove that they don’t owe money.
The government said the new healthcare matching scheme is meant to prevent and identify fraudulent and incorrect Medicare claiming. The proposed legislation amends the National Health Act and Health Insurance Act to enable data-matching for Medicare compliance purposes.
“Improved data-matching capabilities supported by the proposed legislative changes will assist the department to more efficiently and accurately detect fraud, incorrect or inappropriate claiming to ensure a greater percentage of incorrect paid benefits are identified and recovered,” the government said in the consultation guide.
“The changes focus only on improving the department’s ability to match and share data for the purposes of identifying fraud and incorrect or inappropriate claiming.
“The proposed changes will not authorise the automation of compliance outcomes or raising of debts, and the department’s compliance officers will continue to follow prescribed and / or legislated compliance processes.”
The scheme would allow the sharing of specific datasets with Australian government agencies to identify fraudulent or incorrect claims. Current laws allow for data-matching of Medicare Benefits Schedule (MBS) and the Pharmaceutical Benefits Scheme (PBS) in “narrow circumstances”.
The changes will greatly expand this scheme, allow for data from the MBS, PBS, Department of Veteran Affairs, Home Affairs, AHPRA and TGA, with the government also considering include private health insurers providing data on a voluntary basis.
But the consultation guide said that any automation of debts or compliance activities without human oversight – a key issue with the robo-debt scheme – will be “out of scope”.The draft legislation is not final, and the government will be accepting submissions on it until 11 October.
Medicare fraud and incorrect claims are correctly detected mainly through tip-offs and data analysis of existing datasets, but this is very limited in scope, the government said.
“If only one half of a percent of Medicare payments are fraudulently, incorrectly or inappropriately billed, around $180 million of health benefits would be lost that could have otherwise contributed to essential health services for Australians,” it said.
Do you know more? Contact James Riley via Email.

